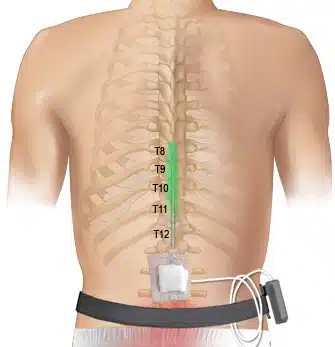
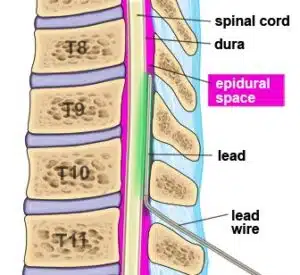
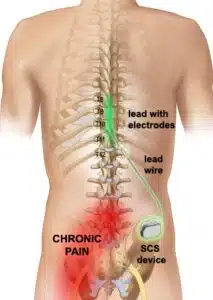
This treatment is an effective alternative to opioid medication and traditional chronic pain therapies. SCS Therapy directs mild electrical pulses that modify or block nerve activity in a non-medicinal way to minimize the sensation of pain reaching the brain. This stimulation has similarities to a cardiac pacemaker, leading some to call the device a pacemaker for pain.
Spinal Cord Stimulator provides medication-free, ongoing pain management and control with a relatively minor, minimally-invasive surgical procedure. Instead of taking a medication that affects the whole body and causes sleepiness, constipation, or other problems unrelated to the pain, spinal cord stimulation delivers pain relief only where it is needed. This therapy is also completely reversible. If you decide at any time to discontinue the therapy, the wires and generator can be removed without permanent damage to the spine.