Procedures
Dekompressor Discectomy
Dekompressor Discectomy Is an Effective Procedure Used to Preserve or Restore Neurological Function, Stabilize Spinal Segments, Improve Functional Status, and Relieve Pain. To Learn More About Dekompressor Discectomy
 WHAT IS A DEKOMPRESSOR DISCECTOMY?
WHAT IS A DEKOMPRESSOR DISCECTOMY?
This minimally-invasive procedure uses a small needle and probe device to reduce a herniated disc, quickly relieving pain in most patients. The procedure may be performed on an outpatient basis using a gentle, relaxing medicine and local anesthetic.
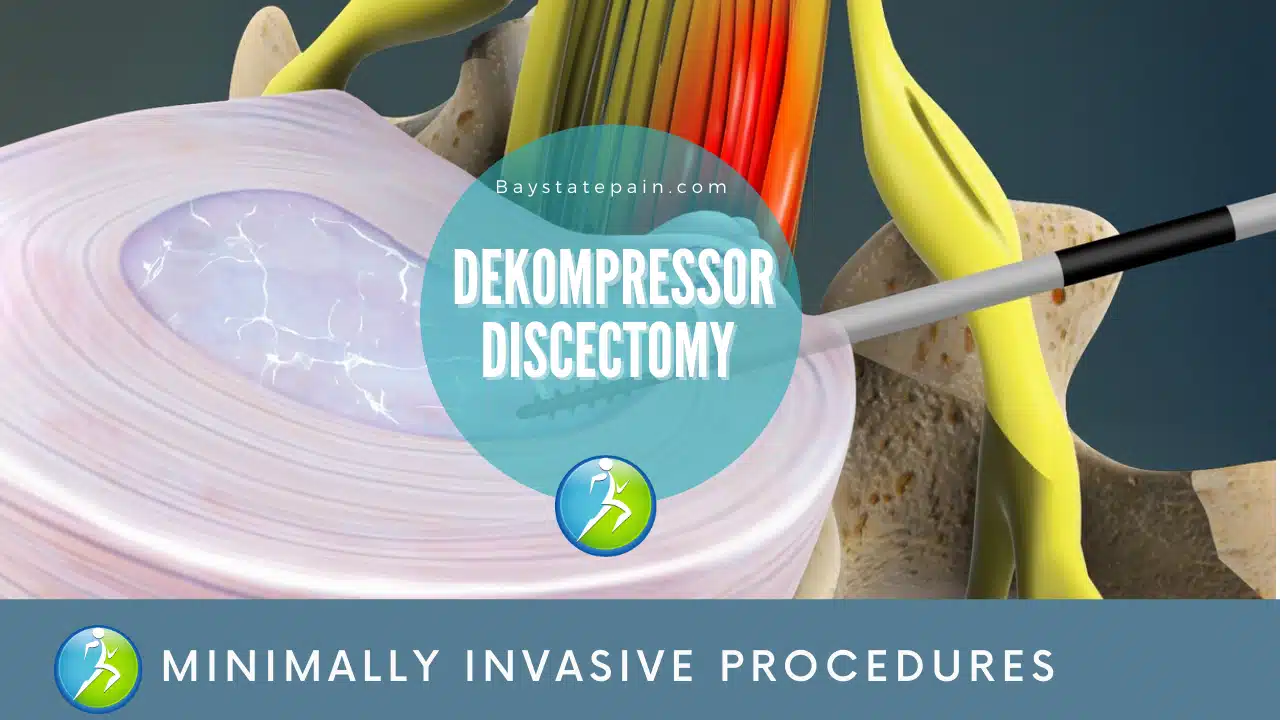
A Dekompressor Discectomy removes part of a herniated disc because it is irritating a nerve and causing pain. In this minimally invasive procedure, a small needle is advanced to the herniated disc guided by a fluoroscope. A probe with a rotating tip is then inserted through the needle to reach the herniated disc.
When the probe is turned on, its tip drills away part of the disc nucleus, creating space for the herniated disc wall and relieving pressure on the nerve. The dekompressor discectomy is used to preserve or restore neurological function, stabilize spinal segments, improve functional status, and relieve pain.
CANNULA INSERTED
After some anesthetic is injected to numb the area, a thin needle called a cannula is inserted through the back and into the herniated disc. The surgeon uses x-ray images to guide the placement of the cannula.
DISC NUCLEUS TREATED
The small probe is carefully inserted through the cannula and into the disc. When the probe is turned on, its rotating tip removes small portions of the disc nucleus. Because only enough of the disc is removed to reduce pressure inside the disc, the spine remains stable.
HERNIATION RELIEVED
The empty space created by the probe allows the disc to reabsorb the herniation.
If you are considering discectomy surgery to relieve pain from a herniated disc, it’s completely understandable that you may have concerns about the risk of reherniation. Being aware of risk factors and exploring the possibility of an annular closure device may decrease the likelihood of reherniation, recurring symptoms, and the need for surgery.
 WHAT IS A DEKOMPRESSOR DISCECTOMY?
WHAT IS A DEKOMPRESSOR DISCECTOMY?